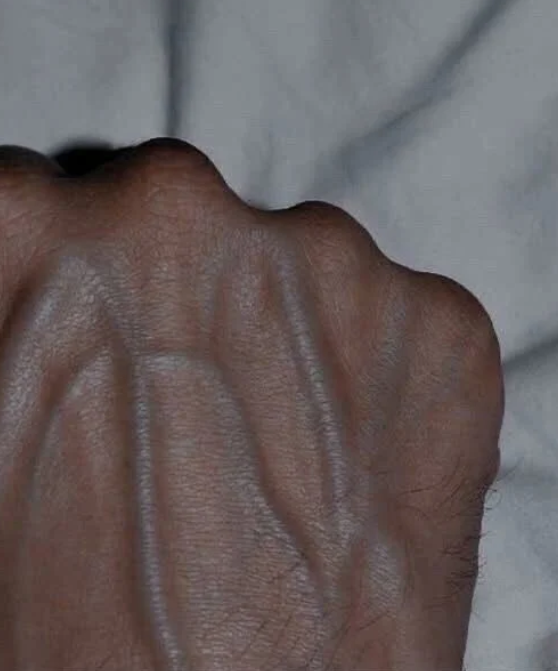
You glance at your hands and notice those blue-green veins popping like a road map under your skin. Maybe you’re a gym buff, and you’re thinking, “Nice, my hard work’s showing!” Or maybe you’re wondering if it’s just age creeping in—or something more serious. Visible veins on your hands, arms, or legs are usually no big deal, but sometimes they’re waving a flag you shouldn’t ignore. Let’s dive into why your veins might be stealing the spotlight, what’s harmless, and when it’s time to call a doctor. Spoiler: It’s not always about those bicep curls.
Why Are My Veins So Visible?
First off, prominent veins are often just your body doing its thing. If you’re lean, athletic, or just getting older, your veins might be more noticeable. Low body fat—think under 15% for men or 20% for women—means less padding to hide those blood highways, especially in places like your hands or forearms. Athletes, especially weightlifters or runners, often sport veiny arms due to boosted blood flow and muscle pump, a badge of their grind. Aging plays a role too: As skin thins with time (collagen production drops about 1% yearly after age 30), veins peek through more clearly.
Even genetics can make your veins stand out. Some folks naturally have thinner skin or more superficial veins, giving that vascular look without breaking a sweat. Hot weather, a post-workout flush, or even dehydration can also make veins pop temporarily by increasing blood flow or shrinking tissue around them. Pregnant women might notice veiny hands or legs due to hormonal shifts and extra blood volume—up to 50% more, per the Cleveland Clinic—putting pressure on veins.
But here’s the catch: If your veins suddenly go from subtle to whoa, or they come with pain, swelling, or weird vibes, it’s time to pay attention. Let’s break down the potential culprits.
When It’s More Than Skin Deep
Sometimes, visible veins are your body’s SOS signal. Here are the big ones to watch for, backed by what experts say:
- Chronic Venous Insufficiency (CVI): Picture your veins as one-way streets for blood heading back to your heart. When the tiny valves inside them weaken—often from high blood pressure, obesity, or prolonged sitting/standing—blood pools in your legs. This can make veins bulge, twist, or swell. About 40% of adults deal with some form of CVI, per the Society for Vascular Surgery, and it’s more common in women and those over 50. Symptoms? Achy legs, swelling, or skin changes like darkening or itchiness. Left unchecked, CVI can lead to ulcers or infections, especially near the ankles.
- Varicose Veins: These rope-like, gnarled veins are CVI’s flashier cousin, affecting 1 in 3 adults, per the National Institutes of Health. They’re often cosmetic at first—think blue squiggles on your calves—but can cause heaviness, throbbing, or burning. Risk factors include family history, pregnancy, or jobs where you stand all day (shoutout to teachers and nurses). While not always dangerous, severe cases can signal deeper circulation issues.
- Deep Vein Thrombosis (DVT): This is the scary one. DVT happens when a blood clot forms in a deep vein, usually in the leg, blocking flow like a dam. It’s rare—about 1-2 per 1,000 people annually, per the CDC—but deadly if a clot breaks free and hits your lungs (pulmonary embolism). Signs include sudden swelling, pain (like a pulled muscle), redness, or warmth in one leg. Risk spikes if you’re immobile (think long flights), smoke, use certain meds like birth control, or have conditions like cancer. In 2025, post-COVID clotting concerns have doctors extra vigilant, as studies show lingering inflammation can up DVT odds.
- Other Red Flags: Sudden vein changes could hint at bigger issues. Cardiovascular strain—say, from high blood pressure or heart failure—can stress veins, making them bulge. Liver problems, like cirrhosis, can also cause blood to back up, leading to visible veins (especially in the abdomen). If you’re feeling fatigued, jaundiced, or have unexplained bruising alongside those veins, it’s doctor time.
Real Stories, Real Warnings
Social media’s buzzing with vein talk. On X, users like @HealthBit posted in September 2025: “Noticed my hand veins popping like crazy lately—normal or nah?” Replies ranged from “Just means you’re shredded!” to “Check for DVT, my cousin ignored it and almost died.” A viral TikTok from a nurse practitioner warned, “Bulging veins + leg pain? Don’t Google, get an ultrasound.” These anecdotes echo a 2023 study in the Journal of Vascular Surgery: 20% of patients with new-onset vein prominence had underlying CVI or DVT, often missed until symptoms worsened.
Take Sarah, a 42-year-old marathoner from Wisconsin, who shared her story on a Reddit thread last month. Her veiny calves looked like a runner’s trophy—until swelling and cramps hit. “I thought it was just overtraining,” she posted. A doctor diagnosed early CVI, likely from years of high-impact running and a genetic predisposition. Compression socks and elevating her legs became her new routine, dodging worse outcomes.
What You Can Do: Protect Your Pipes
Good news: Most veiny vibes are manageable, and prevention’s your best friend. Here’s your playbook, straight from vascular pros:
- Move It: Regular exercise—30 minutes most days—keeps blood pumping and veins happy. Walking, swimming, or yoga are gold for circulation. Avoid sitting or standing too long; if you’re desk-bound, do ankle pumps or take 5-minute walk breaks hourly.
- Gear Up: Compression stockings (15-20 mmHg for mild cases) gently squeeze legs, pushing blood upward. They’re a game-changer for CVI or varicose veins, cutting swelling by up to 50%, per a 2024 study in Phlebology. Pregnant? Ask your doc about maternity versions.
- Check In: If veins bulge suddenly, hurt, or come with swelling, redness, or fatigue, see a doctor pronto. An ultrasound can spot CVI or DVT in minutes. For mild varicose veins, treatments like sclerotherapy (injections to collapse veins) or laser therapy are minimally invasive and 90% effective, per the Mayo Clinic.
- Lifestyle Hacks: Stay hydrated, maintain a healthy weight (obesity doubles CVI risk), and quit smoking—it’s a vein constrictor. Elevate legs 15 minutes daily to ease pressure. If you’re pregnant or on hormone therapy, talk to your doc about vein health monitoring.
The Bigger Picture: Listen to Your Body
Visible veins are often just your body’s art, especially if you’re fit, aging, or feeling the heat. But they can also be a whisper—or a shout—from your vascular system. In 2025, with rising obesity rates (42% of U.S. adults, per CDC) and sedentary Zoom-life lingering post-pandemic, vein issues are climbing. Yet awareness lags—only 10% of CVI patients seek treatment early, says the American Vein & Lymphatic Society.
So, next time you spot those veins snaking across your hands or legs, take a beat. Flex your fitness pride, sure, but stay curious. A quick check could keep you striding strong—or save your life. Got pain or swelling? Don’t wait for Google to play doctor. Call a pro, and keep those veins flowing smoothly.